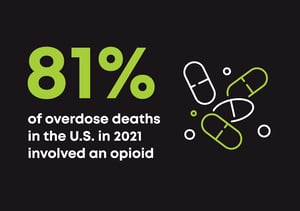
 81% of overdose deaths in the U.S. in 2021 involved an opioid.
81% of overdose deaths in the U.S. in 2021 involved an opioid.
What should be an obvious signal to support widespread opioid use disorder treatment has instead become a forgotten statistic. To make matters worse, we have the proven telehealth treatment options to make an impact, yet access is being hindered by complicated policy changes.
I recently shared my thoughts in an opinion piece for STAT about the harmful effects of new restrictive policies. The DEA’s proposed ruling is one recent threat that has left many wondering what will happen to patient access to medications for opioid disorder (MOUD). The policy would restrict first time OUD patients to just a 30-day supply of MOUD’s like buprenorphine before requiring an in-person evaluation.
Buprenorphine is a known successful treatment option for OUD. And it's potentially even more effective when prescribed via telehealth because it eliminates common barriers, including strict in-person requirements and the stigma that patients can face with in-person visits. Still, the DEA is putting access to this medication at risk. With the policy currently slated to receive a final decision in November, the time is now to safeguard access to buprenorphine by protecting the treatment methods that expand access. Telehealth treatment isn’t just breaking barriers to care; it’s helping save the lives of those struggling with OUD.
Telehealth could be the only path for treatment continuation for some patients
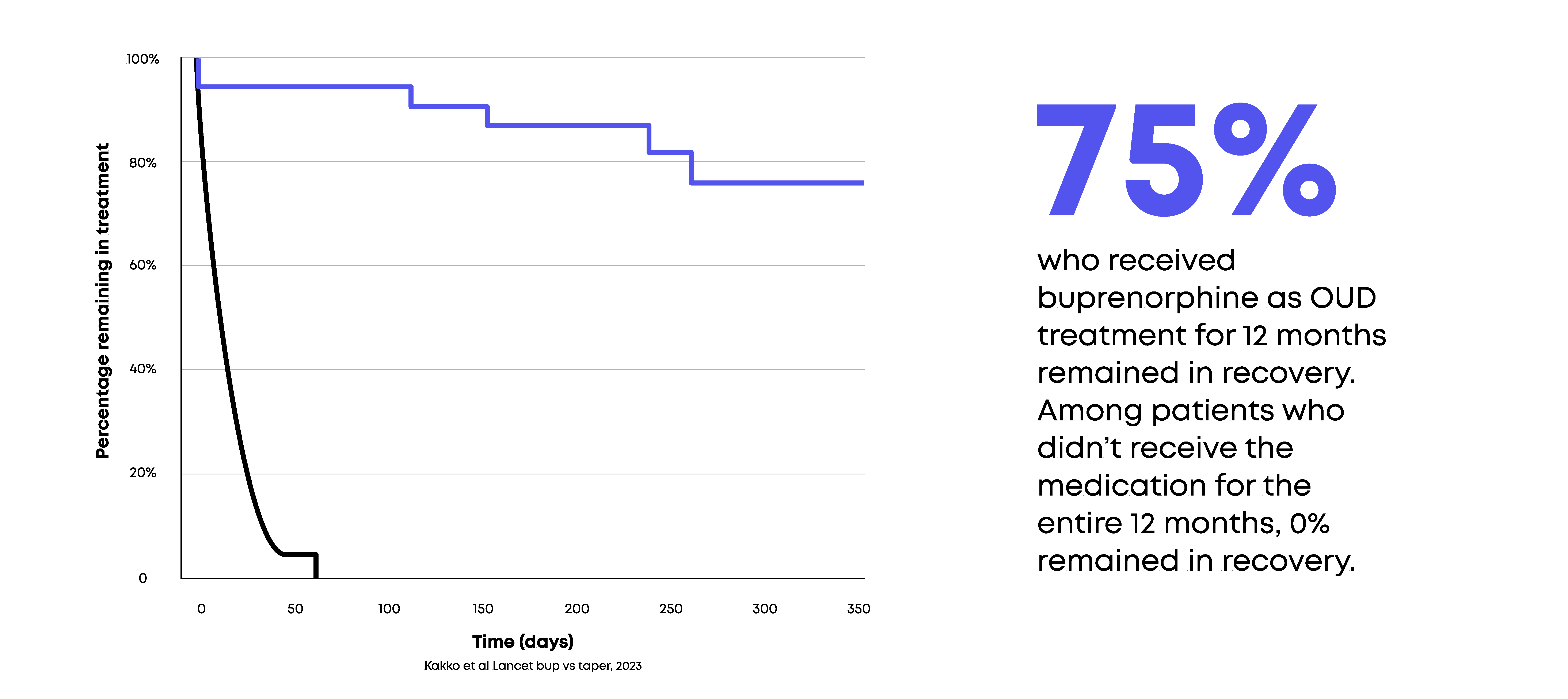
The decision to limit medication access is difficult to understand in the midst of compelling supporting evidence. 75% of patients who received buprenorphine as OUD treatment for 12 months remained in recovery. Among patients who didn’t receive the medication for the entire 12 months, 0% remained in recovery.
Though buprenorphine works, receiving the medication as OUD treatment isn’t as simple as other medications. It requires consistent meetings with a prescriber to ensure appropriate dosing, to monitor patient stability, and to assess progress toward treatment goals. But in many cases, in-person evaluations are logistically difficult and are not necessarily better: telehealth treatment offers patients an easier alternative to accessing effective OUD treatment.
For some, losing their telehealth treatment option—even temporarily—could mean the difference between continuing medication or stopping abruptly with dangerous consequences. OUD patients who are unable to continue buprenorphine treatment are not only at increased risk of visiting the ED and getting hospitalized, they are much more likely to experience overdose and death.
Logistical limitations aren’t the only consideration when it comes to in-person treatment. OUD patients also face societal stigma that deters them from receiving care. National public opinion data revealed that negative attitudes towards those with opioid use disorder are more pervasive compared to other medical conditions, including mental illness. Perhaps more alarming, stigma against people with opioid use disorder is common among those tasked with treating it. According to a 2019 survey, a majority of PCPs were unwilling to have a person taking MOUD as a neighbor or marry into their family.
The DEA is forcing hardships and unnecessary barriers on patients
People with OUD face enough struggle as it is. Additional hardships—like making proven treatment methods more difficult to access—are only doing harm. In the wake of research highlighting telehealth’s undeniable success, it’s clear the DEA’s decision isn’t based on medical necessity; it’s simply another way that we as a society are making it even harder to access OUD treatment for the people whose lives depend on it most.
We should be embracing telehealth by expanding access to crucial medications like buprenorphine and empowering individuals on their path to recovery. As physicians and providers, it’s time to work collectively and protect access to life-saving treatment.