This December, the Supreme Court will determine whether or not the Sackler family (the founders of Purdue Pharma and the makers of OxyContin) can use bankruptcy to shield themselves from criminal liability and prosecution. Marketed as a non-addictive opioid for pain management, OxyContin is the drug that fueled America’s opioid crisis.
The new Netflix docuseries "Painkiller" provides a compelling narrative of the Sacklers' insidious tactics to shift blame onto their victims, labeling opioid use disorder (OUD) as an addiction problem and thereby shielding themselves from blame. It’s easy to call this strategy preposterous (which it is) but it was incredibly effective.
Nearly three decades after Purdue Pharma kicked off America’s opioid crisis, the devastating opioid epidemic now claims 40 lives per day. The media’s focus on the prosecution of the Sacklers is critical. But, I would argue, it's less important than addressing the ongoing and systemic lack of access to effective treatment programs.
When it comes to the opioid crisis, the media and the political class are quick to focus on the criminal prosecution of the Sacklers and preventing fentanyl from crossing our border. Both are fine endeavors, but neither will give a person suffering from opioid use their life back. Neither will increase access to medication, or reduce the stigmatization that these patients face.
America is Still Mislabeling the Victims of the Opioid Crisis
America still sees opioid use disorder (OUD) as an addiction and sees the people who suffer from OUD as drug addicts. Neither statement is factual. Unlike other drugs, opioids frequently alter a patient’s higher brain function to the point that seemingly minor mental health issues, like stress, can trigger withdrawal symptoms (even when opioids have been out of a patient’s system for months) and cause a patient to return to illegal opioid use.
While the Sackler family's role in fueling the opioid epidemic is undeniable, I believe we've missed the mark in our national response by neglecting to focus on making effective and accessible treatment available to every victim of this crisis.
In my daily practice as a physician treating patients with OUD, I witness firsthand the devastating consequences of this mislabeling. My patients, many of whom have endured unimaginable heartbreak and loss, grapple with the stigma associated with their condition and struggle to maintain access to effective medication and treatment.
Despite the immense challenges they face, my patients consistently inspire me with their resilience and unwavering hope. They find joy in simple things like sobriety, friendship, and restored relationships, reminding me of what truly matters in life.
Bipartisan Leadership Has Arrived. Will We Follow It?
The TREATS Act, a bipartisan bill reintroduced in late 2023, offers a beacon of hope in addressing the opioid crisis. It aims to permanently remove regulatory barriers to telehealth-based medication for OUD (MOUD) treatment programs, expanding access to this proven and effective treatment modality.
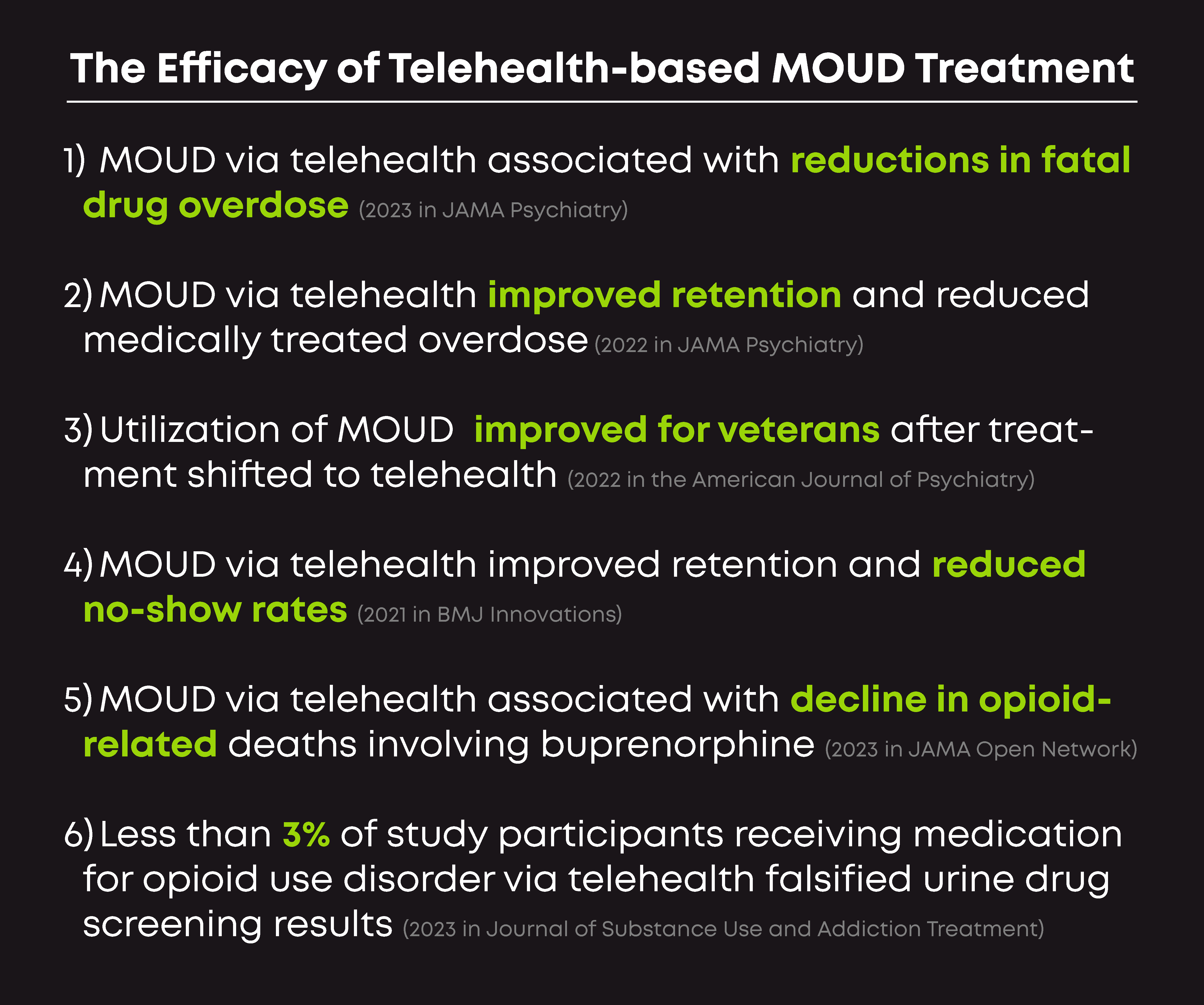
If there were mountains of research showing that increasing access to telehealth-based OUD treatment programs had a negative impact on patients, it might make sense to slow-walk a bill like this. But the opposite is true: since the COVID-19 pandemic made access to MOUD available through telehealth, treatment outcomes have improved.
Here’s just a sample of the research on the efficacy of telehealth-based MOUD treatment programs:
In spite of the nation’s obvious crisis, there is no rush on Capitol Hill to pass and sign the TREATS Act. Instead, TREATS’ impressive list of bipartisan sponsors wades through campaign speeches about putting Americans first, while states continue to move in the opposite direction, throwing up barriers to virtual MOUD care. Restrictive anti-telehealth-based MOUD laws in states like Alabama and Michigan seem to be motivated by protecting entrenched in-person treatment programs as opposed to what's best for patients.
Who Benefits the Most from the TREATS Act
Passage of TREATS is particularly critical for lower-income communities and patients within the criminal justice system. Nearly 3% of the U.S. population suffers from OUD, but prevalence is twice as high in low-income communities, and five times as high among the incarcerated population.
For these people, traditional on-site and in-patient treatment programs are often not realistic options because they’re expensive, hard to reach by public transit, and often don't take insurance (certainly not Medicaid). Certainly, for my working-class patients, in-patient treatment programs that require them to take days, weeks, or months off of work are not an option.
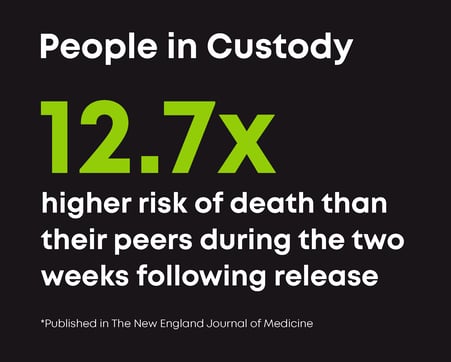
The problem is particularly acute for people with OUD who are released from custody without access to MOUD treatment. These patients face particularly high risks of recidivism, relapse, overdose, and death. A study found that people with OUD in custody had a risk of death 12.7 times higher than their peers during the two weeks following release.
Telehealth-based OUD treatment offers several advantages over traditional in-patient programs, including:
- Flexibility: Telehealth can reach patients in custody settings, overcoming transportation and logistical barriers.
- Treatment continuity: Telehealth ensures seamless care continuity upon release, preventing relapse.
- Effectiveness: Telehealth allows for more frequent and personalized care, enhancing treatment outcomes.
While prosecuting the Sacklers is necessary for accountability, it's crucial to focus on providing effective and accessible treatment for the victims of the opioid crisis. Supporting the TREATS Act is a step towards ensuring that long-term, effective, convenient, and affordable OUD treatment options are available to all who need them.





